Introduction to Modern Healthcare Trends
The landscape of healthcare is undergoing a significant transformation, driven by innovation that addresses the sector’s diverse challenges. This evolution is not just a response to current demands but a proactive move toward a more efficient, personalized, and accessible future in healthcare. Central to these changes are technological breakthroughs and strategic policy shifts that are reshaping how care is delivered and experienced.

Image source: Source
One key driver of these changes is the integration of cutting-edge technologies such as biotechnology, which plays a crucial role in developing novel treatments and enhancing patient care. Organizations like the Biotechnology Innovation Organization (BIO) are leading the way by creating environments where innovation thrives and patient outcomes are prioritized. The BIO 2024 Sessions highlight the important role biotechnology plays in modern healthcare.

Image source: Source
However, innovation brings its own set of challenges. The healthcare sector must carefully navigate these to ensure that advancements do not outpace ethical considerations or worsen existing disparities. As we explore the current trends, it is essential to examine both the benefits and potential pitfalls of this rapid evolution. How can we balance cutting-edge innovation with the foundational principle of “do no harm”? What steps are necessary to ensure new technologies are accessible to all, rather than widening the socioeconomic gap?
This exploration provides a foundation for a comprehensive examination of the innovative trends shaping healthcare today. From artificial intelligence in diagnostics to policy reforms aimed at improving healthcare delivery, each development offers a glimpse into a future where healthcare is more responsive to individual and societal needs. As we proceed, it is important to engage with these trends critically, considering both their transformative potential and the challenges that must be addressed to fully realize their benefits.
Harnessing AI and Personalized Medicine
In the evolving landscape of healthcare, the integration of artificial intelligence (AI) and personalized medicine marks a transformative shift towards precision and efficiency. This convergence is particularly impactful in chronic disease management, where AI’s capabilities are harnessed to tailor treatments to individual patient profiles. AI’s potential lies in analyzing vast datasets, revealing patterns and insights previously inaccessible. This capability is pivotal in developing personalized treatment plans that consider a patient’s unique genetic, environmental, and lifestyle factors.
AI’s application in clinical imaging stands out as a promising advancement in personalized medicine. AI algorithms enhance diagnostic accuracy by identifying subtle patterns in medical images that may be overlooked by human eyes. For instance, in cancer, AI assists in detecting early signs, improving prognosis and treatment outcomes. The integration of AI with imaging technologies not only enhances diagnostic precision but also accelerates the process, enabling timely interventions.
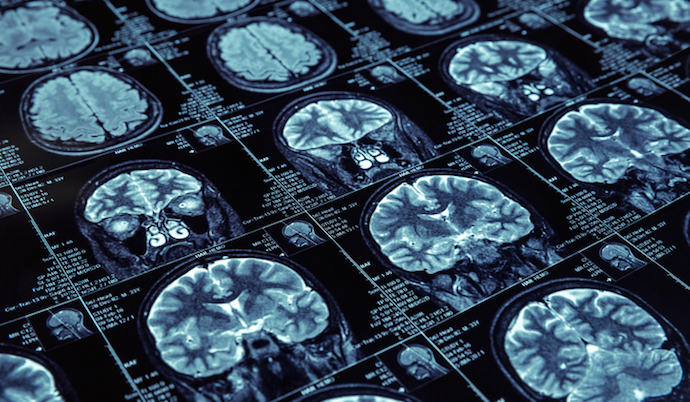
Image source: Source
The Biotechnology Innovation Organization (BIO) emphasizes the importance of these advancements. Through their support, the healthcare sector is witnessing a paradigm shift towards more personalized and data-driven care models. These innovations promise to redefine patient care by ensuring that treatments are effective and specifically tailored to individuals, reducing the trial-and-error approach of traditional medicine. Learn more.
However, the implementation of AI in healthcare presents challenges. Issues such as data privacy, ethical considerations, and the need for regulatory frameworks to ensure patient safety are critical. The reliance on AI systems necessitates a robust technological infrastructure and continuous updates to maintain accuracy and reliability. As we look to the future, AI’s potential in personalized medicine is vast, but its success hinges on addressing these challenges and ensuring equitable access to advancements.
Speculatively, how might AI’s integration reshape the patient-doctor relationship in the coming years? Could AI-driven personalized medicine lead to the eradication of some chronic diseases? While the answer remains uncertain, current developments suggest we are on the brink of a new era in healthcare, where the synergy between AI and personalized medicine could become the cornerstone of modern medical practice. The journey is complex, but the promise of truly personalized healthcare is both exciting and inspiring.
Tackling Economic Challenges in Healthcare
The rising tide of medical costs presents a formidable challenge to healthcare systems worldwide, impacting everything from patient affordability to institutional sustainability. As noted in PwC’s analysis, medical costs are projected to escalate through 2023 and 2024, exerting pressure on both providers and patients. This surge necessitates innovative economic models, such as value-based care, which shifts the focus from volume-based service delivery to patient outcomes.

Image source: Source
Value-based care, a model gaining traction, aims to align healthcare providers’ incentives with patient health outcomes, potentially reducing unnecessary spending. It encourages a holistic view of patient care by integrating preventative measures and chronic disease management. However, transitioning to such models requires overcoming significant hurdles, including restructuring payment systems and ensuring accurate outcome measurement.
Beyond model adoption, the integration of technology, such as AI and data analytics, can optimize resource allocation and improve predictive capabilities for patient care needs. Embracing these technologies could lead to more efficient operations and reduced costs, though the initial investment and system integration pose substantial barriers.
The evolution of economic models in healthcare is likely to be shaped by a combination of policy initiatives and technological advancements. Policymakers can incentivize innovation and support infrastructure changes essential for value-based care implementation. Meanwhile, technological innovations that enhance data interoperability and patient engagement could further alleviate financial pressures by improving care coordination and reducing redundancy.
Will these solutions suffice to curb the relentless rise in healthcare costs? While promising, each comes with its own set of challenges and uncertainties. The future of healthcare economics may well depend on a balance of innovation, policy support, and the adaptability of healthcare systems to embrace new paradigms. As stakeholders navigate these complexities, the ongoing dialogue between economic efficiency and patient-centric care remains crucial.
Improving Efficiency and Addressing Labor Challenges
The modern healthcare landscape faces the critical task of enhancing efficiency while tackling significant labor challenges. These demands are driven by an aging population, increasing patient loads, and the urgent need to deliver high-quality care swiftly and effectively. To meet these demands, technological innovations and strategic workforce management emerge as essential components.
Automation and data analytics play a crucial role in streamlining administrative processes, reducing human error, and enabling healthcare professionals to focus more on patient care rather than paperwork. Artificial intelligence (AI) helps optimize scheduling, manage patient flow, and assist in diagnostics, significantly reducing wait times and operational costs. According to a report by Philips, these technologies are current trends reshaping healthcare delivery.

Image source: Source
However, the integration of advanced technologies necessitates upskilling the current workforce, which can be resource-intensive. There is also concern over technology displacing jobs, adding complexity to workforce management strategies. To counter these challenges, healthcare systems are adopting flexible workforce models. These include telecommuting for administrative tasks, employing part-time or contract workers to meet peak demands, and investing in continuous education programs to keep the workforce adept at handling new technologies.
Labor shortages in healthcare are exacerbated by international migration patterns, with skilled professionals moving to more developed countries for better opportunities, leaving a gap in low-income regions. This trend calls for a global effort in sustainable workforce planning. The World Health Organization emphasizes creating attractive working conditions and career paths to retain talent locally while fostering international collaboration to share best practices and resources.
As healthcare systems navigate these complex dynamics, balancing the integration of advanced technologies with effective workforce management is critical to ensuring sustainable, high-quality healthcare delivery. This synergistic approach not only addresses current inefficiencies but also prepares healthcare systems for future challenges.
Technological Advancements Shaping Healthcare Delivery
In the ever-evolving realm of healthcare, technology is reshaping how services are delivered. Telemedicine, artificial intelligence (AI), and 3D printing are at the forefront of this transformation, each offering unique contributions to the healthcare landscape.
Telemedicine has swiftly transitioned from a novel concept to a fundamental component of modern healthcare. Today’s telemedicine platforms enable real-time consultations, remote monitoring, and virtual diagnostic procedures. This convenience and accessibility have revolutionized patient engagement, particularly in remote or underserved areas. The future may see further integration with wearable technology, allowing for continuous health monitoring and potentially reducing the need for frequent hospital visits.
Artificial intelligence is another cornerstone driving change. AI’s capacity for data analysis and pattern recognition enhances diagnostics, predicts patient outcomes, and tailors individualized treatment plans. This integration promises to improve accuracy and efficiency while supporting healthcare professionals in making informed decisions. However, as AI systems become more integrated into clinical settings, considerations regarding data privacy and the ethical implications of machine-led decisions will be essential.
Meanwhile, 3D printing is revolutionizing the design and production of medical devices and prosthetics. This technology allows for the creation of highly personalized medical solutions, tailored to specific anatomical needs. Advancements in biocompatible materials enable new possibilities for patient-specific implants and reconstructive surgery. The potential for 3D printing in drug development, with the ability to print personalized medication doses, hints at a future where treatments are as unique as the individuals receiving them.
These technologies are not just enhancing existing healthcare delivery methods; they are paving the way for new paradigms in patient care. The Innovative Health Initiative plays a pivotal role in fostering these advancements, ensuring that the future of healthcare is not only innovative but also inclusive and accessible.
Navigating Cybersecurity in Healthcare
As digital transformation sweeps through healthcare, the sector finds itself at a precarious intersection of innovation and vulnerability. In 2024, there has been a notable escalation in cyberattacks targeting healthcare institutions, demonstrating the potential to disrupt critical services and compromise sensitive patient data. This underscores the urgency for robust cybersecurity measures.

Image source: Source
The healthcare industry, rich in sensitive information, has become a prime target for cybercriminals. The American Hospital Association highlights a surge in ransomware attacks, which jeopardize patient safety and strain the financial and operational capabilities of healthcare providers. As healthcare systems continue to digitize, the attack surface expands, offering more opportunities for cyber adversaries. Healthcare leaders must prioritize cybersecurity resilience to protect against evolving threats, as suggested in a recent report by the AHA.
The challenge intensifies as healthcare systems integrate advanced technologies like AI and IoT devices. While transformative, these technologies introduce new risks. How can healthcare institutions balance the benefits of these technologies with the necessity for secure data environments? This question looms large as the sector navigates the line between innovation and security.
Strategies for safeguarding sensitive healthcare data must evolve with these technological advancements. Embracing a multi-layered security framework—including encryption, access controls, and continuous monitoring—can bolster defenses against cyber threats. Moreover, fostering a culture of cybersecurity awareness among healthcare professionals is crucial. This approach mitigates risks and empowers staff to recognize and respond to potential threats proactively.
Regulation and policy play a significant role in shaping cybersecurity practices. As legislators work to keep pace with technological change, developing international cybersecurity standards could provide a unified approach to managing cyber risks globally. Healthcare institutions must stay informed and adaptable, ensuring that their cybersecurity strategies align with emerging threats and technological trends.
The road ahead in cybersecurity for healthcare is challenging yet presents opportunities for innovation and collaboration. By advancing robust cybersecurity measures, the healthcare sector can safeguard its digital future, ensuring that technological innovation does not compromise patient trust and safety.
Global Healthcare Trends and Workforce Dynamics
The global healthcare landscape is continuously shaped by multifaceted trends, with workforce migration standing as a pivotal aspect. This movement of healthcare professionals across borders is driven by factors such as economic incentives, career opportunities, and geopolitical conditions. It presents a double-edged sword, particularly impacting low-income countries where the departure of skilled healthcare workers can exacerbate existing shortages, ultimately affecting healthcare delivery and patient outcomes. According to the World Health Organization, the international migration of health workers significantly challenges sustainable workforce planning, highlighting the urgent need for coordinated global policies to address these imbalances. Read more from WHO.
The anticipated global health challenges require a nuanced approach to workforce dynamics. Issues such as aging populations, the prevalence of chronic diseases, and the emergence of pandemics demand a robust and adaptable healthcare workforce. This necessitates international cooperation and strategic planning to ensure that health systems are resilient and capable of meeting future demands. Developing global frameworks for workforce sustainability is crucial, emphasizing capacity-building initiatives in regions most vulnerable to workforce depletion.
Moreover, as healthcare systems worldwide increasingly rely on technology and digital innovations, there’s a critical need to invest in training and development programs for healthcare professionals. This ensures they possess the necessary skills to integrate emerging technologies into their practice effectively. The intersection of technology and healthcare workforce dynamics not only promises enhanced patient care but also poses questions about the future role of healthcare workers in an increasingly automated environment. How prepared are healthcare systems for a landscape where artificial intelligence and machine learning play significant roles in diagnosis and treatment?
Addressing these global healthcare trends and workforce dynamics is imperative for fostering a resilient healthcare system capable of withstanding future challenges. International cooperation, strategic workforce planning, and the integration of technology are key components in navigating this complex landscape, ensuring that healthcare systems globally are equipped to deliver equitable and efficient care to all populations.
Wearable Technology and Health Equity
Wearable technology has emerged as a pivotal player in modern healthcare, offering opportunities to bridge gaps in healthcare access and inclusivity. Devices such as smartwatches and advanced health monitors aim to democratize health data access, enabling individuals across various socio-economic backgrounds to monitor and manage their health more effectively. Recent advancements in wearable tech highlight their growing role in chronic disease management, providing real-time data collection and personalized insights that empower users to take control of their health.

Image source: Source
Wearable devices significantly impact individuals with chronic conditions by allowing for remote monitoring of heart rate, glucose levels, and physical activity. This capability provides critical data that can lead to timely interventions, reducing the need for frequent in-person medical visits. Such technology is particularly beneficial for those in remote or underserved areas, where healthcare resources are limited, offering a lifeline to those who might otherwise lack access to continuous care.
However, achieving health equity through wearable technology presents challenges. The cost of these devices can be prohibitive, necessitating initiatives to subsidize or reduce their cost and make them affordable to a broader audience. Additionally, the technology must be designed with diverse populations in mind, ensuring it is user-friendly and adaptable to different needs and preferences.
Looking ahead, wearable technology holds promising potential for further advancing health equity. Innovations such as integration with artificial intelligence (AI) for sophisticated health analytics and the development of non-invasive sensors for comprehensive health monitoring could revolutionize personal health management. As wearable technologies evolve, partnerships between tech companies, healthcare providers, and policymakers will be crucial in addressing barriers to accessibility and crafting solutions that place health equity at the forefront.
Policy Changes and Legislative Developments
In recent years, healthcare policy has undergone substantial changes, especially in telehealth and the integration of artificial intelligence (AI). These shifts are transforming healthcare access and delivery, reflecting a dynamic regulatory landscape that aims to keep pace with technological advancements.
Telehealth, once a supplementary service, has become a cornerstone of modern healthcare policy. The expansion of Medicare telehealth services underscores a commitment to enhancing access to remote medical care. This policy shift is crucial in bridging geographical barriers and ensuring that patients receive timely medical consultations, irrespective of their location. Such regulatory adaptations are increasing healthcare accessibility and pushing healthcare systems to innovate further in digital health solutions.
Alongside telehealth, AI integration into healthcare systems is another significant policy focus. AI’s potential to revolutionize diagnostics and treatment protocols necessitates reevaluating existing regulatory frameworks. Policymakers must balance innovation with ethical considerations, ensuring AI technologies are used responsibly and equitably. This involves setting standards for data privacy, algorithm transparency, and bias mitigation to maintain public trust and enhance patient outcomes.
Future policy trends are likely to emphasize interoperability and data sharing across platforms to facilitate seamless care delivery. As healthcare systems become increasingly digital, regulatory bodies may focus on creating unified standards that support the secure and efficient exchange of patient information. This could enhance collaborative care models and improve patient outcomes through integrated care pathways.
Moreover, the push towards value-based care aligns with legislative efforts to reform payment models, rewarding healthcare providers for quality rather than quantity of care. This shift aims to contain rising medical costs while improving patient satisfaction and outcomes, a topic that requires ongoing legislative attention to ensure equitable implementation and sustainability.
As the healthcare sector continues to evolve, it is essential to consider how these policy changes will shape the future of healthcare delivery. Will they fully realize the potential benefits of technological integration, or will new challenges emerge that require further legislative intervention? The coming years will be pivotal in defining the trajectory of healthcare policy and its impact on global health systems.
Exploring Future Healthcare Trajectories
As healthcare technology evolves, the future of the industry holds exciting possibilities yet uncharted. One emerging area is quantum computing, which promises to revolutionize data security and processing speeds in healthcare, potentially transforming how patient data is handled and safeguarded. This innovation could address some of the pressing cybersecurity challenges highlighted in previous sections by providing unbreakable encryption methods and rapid data analysis capabilities.
Image source: Source
Moreover, the integration of cutting-edge biotechnological advancements, such as CRISPR gene editing, offers the potential to tackle previously untreatable diseases. These technologies not only push the boundaries of medical treatment but also raise ethical questions about the extent of human intervention in natural processes. How will society balance the benefits and ethical considerations of such powerful tools?
Looking ahead, the healthcare sector must also consider the implications of these advancements on workforce dynamics. As automation and technology change the landscape, how will the roles of healthcare professionals evolve? These questions highlight the need for adaptive strategies and policies that ensure a balanced integration of technology while maintaining human-centric care.
Engaging with these emerging trends and contemplating their broader impacts will be crucial for both healthcare providers and patients. As these technologies continue to develop, staying informed and proactive will be essential for navigating the future of healthcare effectively.
