From Needles to Pills: A New Era in Diabetes Treatment
Imagine a world where managing diabetes is as easy as taking a daily vitamin. The transition from injectable to oral GLP-1 receptor agonists is revolutionizing diabetes treatment, making it far more convenient and accessible for patients. For many, needles have long been a dreaded part of their routine. But now, thanks to scientific advances, the fear of injections might soon become a thing of the past.

Image source: Source
This shift is significant due to its impact on accessibility and ease of use. Not everyone is comfortable with needles, and the thought of regular injections can be daunting. Oral medications offer a hassle-free alternative that fits seamlessly into daily life. These pills are opening doors for patients who previously struggled with adherence to their treatment plans. The simple act of swallowing a pill, rather than preparing an injection, can significantly enhance one’s willingness to stick with the prescribed regimen.
Beyond convenience, this transition also aims to improve health outcomes. Easier treatment methods lead to better adherence, resulting in more consistent therapy and improved management of the condition. This can translate into fewer complications and a higher quality of life. According to a study on the transition of peptide GLP-1 receptor agonists from injection to oral delivery, this change is a promising step forward in diabetes care.
Moving from needles to pills marks a significant milestone in diabetes treatment. It simplifies the process and empowers patients to take control of their health with more confidence and less anxiety. The future of diabetes management is already here, making life easier for many.
What Are GLP-1 Receptor Agonists and Why Do They Matter?
Think of your body as an orchestra, with GLP-1 receptor agonists acting as the conductors ensuring everything runs smoothly, especially in managing type 2 diabetes.
GLP-1, or Glucagon-Like Peptide-1, is a hormone that significantly contributes to blood sugar regulation. Upon eating, GLP-1 is released from the intestines, signaling the pancreas to produce insulin. Insulin facilitates the uptake of glucose into cells for energy. Additionally, GLP-1 slows the movement of food through the stomach, allowing for better nutrient absorption and stable blood sugar levels.
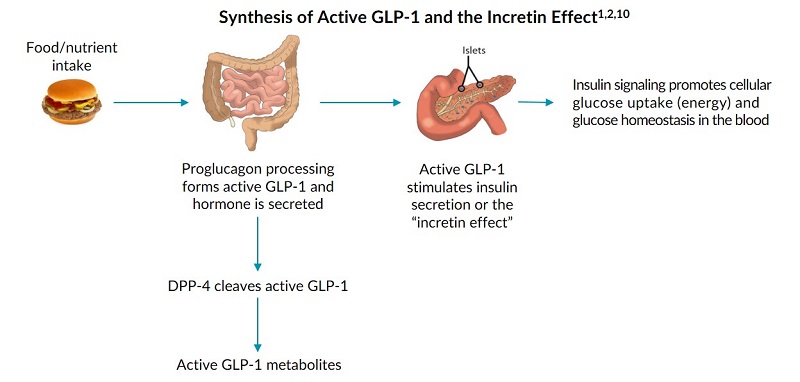
Image source: Source
In type 2 diabetes, the body either lacks sufficient insulin or resists its action, resulting in high blood sugar levels. GLP-1 receptor agonists mimic natural GLP-1, enhancing insulin production and glucose management. They also support weight management by promoting satiety and reducing appetite, which is crucial for those with type 2 diabetes who often struggle with obesity.
The transition of GLP-1 receptor agonists from injectable to oral forms is transformative, simplifying treatment and improving adherence. This change not only offers convenience but also broadens the accessibility of these medications, potentially benefiting many managing type 2 diabetes. According to a recent study, this shift could significantly enhance treatment success.
GLP-1 receptor agonists are more than just another treatment option; they represent hope and improved health outcomes, especially with the advancements in oral delivery methods.
The Science Behind the Pill: Overcoming Delivery Challenges
Imagine trying to deliver a message in a bottle, but the ocean’s waves keep smashing it against the rocks. That’s similar to the challenge of transforming GLP-1 receptor agonists—important medicines for managing type 2 diabetes—from injections into pills. The journey from the stomach to the bloodstream is fraught with obstacles, but research is making headway in addressing these issues.

Image source: Source
A significant hurdle in creating oral GLP-1 receptor agonists is ensuring the medication remains stable in the stomach’s harsh environment, filled with strong acids that can break down the medicine before it reaches the intestines. Scientists are developing special coatings and formulations that protect the medicine as it travels through the stomach, ensuring it remains intact until it reaches the right part of the digestive system.
Once past the stomach, absorption is the next challenge. The medicine needs to pass through the intestinal walls into the bloodstream to be effective. However, the large size and complex structure of GLP-1 receptor agonists make absorption difficult. Researchers are experimenting with techniques, such as using absorption enhancers that temporarily open pathways in the intestine walls, allowing the medicine to pass more easily.
Another approach involves designing molecules that mimic the natural pathways used by nutrients to enter the bloodstream. This requires a deep understanding of nutrient absorption and cleverly engineering the medicine to hitch a ride on these pathways. These advancements hold promise for transforming how we take these medications, moving from needles to pills.
Innovative research is continuously pushing boundaries as scientists develop new technologies to overcome these delivery challenges. Advances in nanotechnology, for instance, are being explored to create tiny carriers that transport the medicine directly to where it’s needed, bypassing obstacles along the way.
By overcoming these delivery challenges, oral GLP-1 receptor agonists are becoming a more viable and convenient option for patients, representing a significant leap forward in diabetes care and offering hope for improved patient compliance and outcomes. For those interested in diving deeper into the science driving these breakthroughs, you can explore more detailed studies on the topic, such as the research published by Frontiers.
Breakthroughs and Approvals: The Latest Milestones
Imagine managing diabetes with the simplicity of taking a daily vitamin. This vision is becoming reality with the FDA’s approval of oral semaglutide, a groundbreaking advancement in diabetes care. This pill marks a significant shift from traditional injections, offering a more comfortable and accessible option for many patients.

Image source: Source
Why is this development so crucial? Transitioning to oral medication not only enhances convenience but also improves patient adherence. People generally prefer swallowing a pill to dealing with needles, which can significantly boost their commitment to treatment plans and lead to better health outcomes.
The journey to develop oral semaglutide involved overcoming complex challenges, such as ensuring the medication’s effectiveness despite the stomach’s harsh environment. Pioneering technology now allows the active ingredients to reach the bloodstream intact, a testament to years of dedicated research.
Pharmaceutical companies continue to explore new frontiers in oral drug delivery, with numerous clinical trials testing innovative formulations. These efforts aim to refine medications, making them even more effective and widely accessible. The relentless pursuit of advancement in this field not only promises to ease diabetes management but also sets a precedent for other complex therapies.
For those interested in the detailed journey of oral semaglutide from concept to market, the NCBI Bookshelf offers a comprehensive overview of the milestones achieved in this remarkable transformation.
Pills vs. Needles: Which Is Better?
When managing type 2 diabetes, the choice between pills and needles can be crucial. Both oral and injectable GLP-1 receptor agonists are effective in controlling blood sugar levels and aiding weight loss, essential elements in diabetes management. The decision often hinges on personal preference and lifestyle.
Oral semaglutide, for example, offers benefits similar to injectable forms and might appeal to those who prefer avoiding needles. A review highlights its potential to improve treatment adherence by eliminating the discomfort associated with injections. This can enhance the overall effectiveness of the treatment plan by ensuring consistent use.
In terms of safety, both oral and injectable GLP-1 receptor agonists are generally well-tolerated, with mild side effects like nausea or diarrhea. These medications require a healthcare provider’s prescription and monitoring to ensure they are used effectively and safely.
The convenience of a once-daily pill can significantly boost patient compliance, as many find it easier to incorporate into daily routines. The psychological benefit of avoiding needles can also be a significant factor, as anxiety or discomfort with injections often hinders regular use.

Image source: Source
Ultimately, the choice between pills and injections is about flexibility and personal preference. Some may opt for injections due to familiarity or because it suits their lifestyle better, while others may find the oral option to be a hassle-free alternative. Consulting with a healthcare provider is crucial to tailoring a treatment plan that aligns with individual needs and health goals. With these options, a personalized approach to diabetes management is achievable.
How Oral Options Enhance Patient Lives
Imagine having a choice between a needle and a pill to take your medicine. For many, this isn’t just about convenience, but a significant improvement in their daily lives. The transition of GLP-1 receptor agonists from injections to oral delivery is reshaping diabetes management, offering a more straightforward and less intrusive method of taking medication.
One of the most remarkable benefits of oral medications is how they boost patient adherence. Oral GLP-1 receptor agonists make diabetes management as easy as taking a daily vitamin, which can be transformative for many people. Handling injections regularly can be daunting and painful, but switching to a pill form removes this barrier, making it easier for patients to maintain their treatment plans consistently. This shift not only improves adherence but also enhances overall treatment outcomes according to research.
The psychological relief of avoiding needles is significant. Many patients report feeling a sense of normalcy and relief when they switch to oral medications. It’s like the difference between wearing a bulky winter coat versus a light jacket. Removing the physical and emotional discomfort of injections allows patients to focus more on living their lives and less on the mechanics of their treatment.
Patient stories highlight the profound impact on their quality of life. People often describe the switch as freeing, allowing them to engage more fully in daily activities without the constant reminder of their condition through injections. This transition emphasizes that medical advancements are not just about treating conditions but also about improving the experience of living with a chronic illness.

Image source: Source
The approval of oral options like semaglutide marks a significant step towards a more patient-friendly approach to diabetes management. This advancement underscores the importance of continuing to innovate in ways that prioritize patient comfort and convenience, ultimately transforming healthcare experiences for the better.
Looking Ahead: The Future of Oral GLP-1 Receptor Agonists
The future of oral GLP-1 receptor agonists in diabetes care is promising, with ongoing advancements poised to enhance their impact. These medications are gaining traction globally, driven by the rising prevalence of diabetes and obesity, indicating a strong demand for more accessible treatment options. According to a study by Global Market Insights, the market for GLP-1 receptor agonists is on an upward trajectory [source].
Research is actively exploring next-generation oral treatments, focusing on improved formulations and expanded therapeutic applications. One exciting area is their potential role in obesity management. Given their dual benefits in controlling blood sugar and promoting weight loss, GLP-1 receptor agonists could significantly broaden their market and therapeutic scope.
Pharmaceutical companies are investing in understanding the long-term effects and benefits of these medications. This includes enhancing their effectiveness and safety, crucial for broader acceptance among healthcare providers and patients. The clinical pipeline remains robust, with numerous trials underway to explore new formulations and combinations that promise greater efficacy and convenience.
These advancements suggest that oral GLP-1 receptor agonists could soon become a cornerstone in managing chronic metabolic conditions. As research and development continue to innovate, these medications are not only improving current treatments but also reimagining the future of metabolic healthcare.

Image source: Source
Imagine a future where managing diabetes is as simple as taking a daily vitamin. This is the direction we’re heading, with oral GLP-1 receptor agonists leading the charge. These advancements are more than just medical innovations—they represent a commitment to improving patient quality of life.
The transition from needles to pills offers hope for an easier, more effective way to manage diabetes. But what does the future hold? As research continues, we anticipate even more groundbreaking developments that could transform diabetes care. Imagine treatments that not only control blood sugar but also address related health issues like obesity.
As these innovations become more mainstream, they highlight a shift toward patient-centered care. This is about aligning treatments with your lifestyle, making it easier to manage your health. The future is bright, and with ongoing research, we can expect more accessible treatment options on the horizon.
Stay informed and join the conversation about these exciting developments. Engage with communities and experts dedicated to diabetes care. Together, we can embrace this new era of innovation, pushing the boundaries of what’s possible in managing diabetes.
